Aetna Breast Pump — Your 2025 Guide to Coverage, Ordering
Aetna plans generally cover a breast pump and lactation support with little to no out-of-pocket cost when you follow in-network steps. This guide explains eligibility, what’s typically covered, how to order through a DME supplier, when hospital-grade rental applies, timelines, common denial reasons (and fixes), plus pro tips to make the process smoother.
How coverage works (ACA basics & plan differences)
Under U.S. preventive-care rules, most non-grandfathered health plans must cover breastfeeding support, counseling, and equipment for the duration of breastfeeding with no cost-sharing when you use in-network providers. Aetna plans implement this benefit, but details can vary by product (HMO, PPO, EPO) and especially by self-funded employer plans. Always verify your specific plan’s Summary of Benefits and Coverage (SBC) and check whether your plan requires a prescription or prior authorization.
Translation: The benefit exists, but the rules you must follow (in-network suppliers, documentation, upgrade allowances) depend on your exact plan.
What Aetna typically covers
- Pumps: A standard manual or standard electric (non-hospital-grade) pump when pregnant or breastfeeding, through an in-network DME supplier.
- Supplies: Tubing, valves, diaphragms, backflow parts, and basic storage supplies—allowances vary by plan and timing.
- Lactation support: Counseling/education with an in-network provider (IBCLC or other covered clinicians) per plan rules.
- Duplication rules: Plans may limit how often you can receive a new electric pump (e.g., once every 12–36 months) and how frequently supplies are covered.
- Upgrades: If you select a pump above your allowance (e.g., premium wearable), many plans will apply the allowed amount and let you pay the difference directly to the DME.
Eligibility & documents checklist
- Active Aetna coverage and member ID
- Estimated due date or baby’s birth date
- Provider’s name and practice info
- Prescription (if required by your plan) — some plans waive this
- Shipping address & contact info for the DME supplier
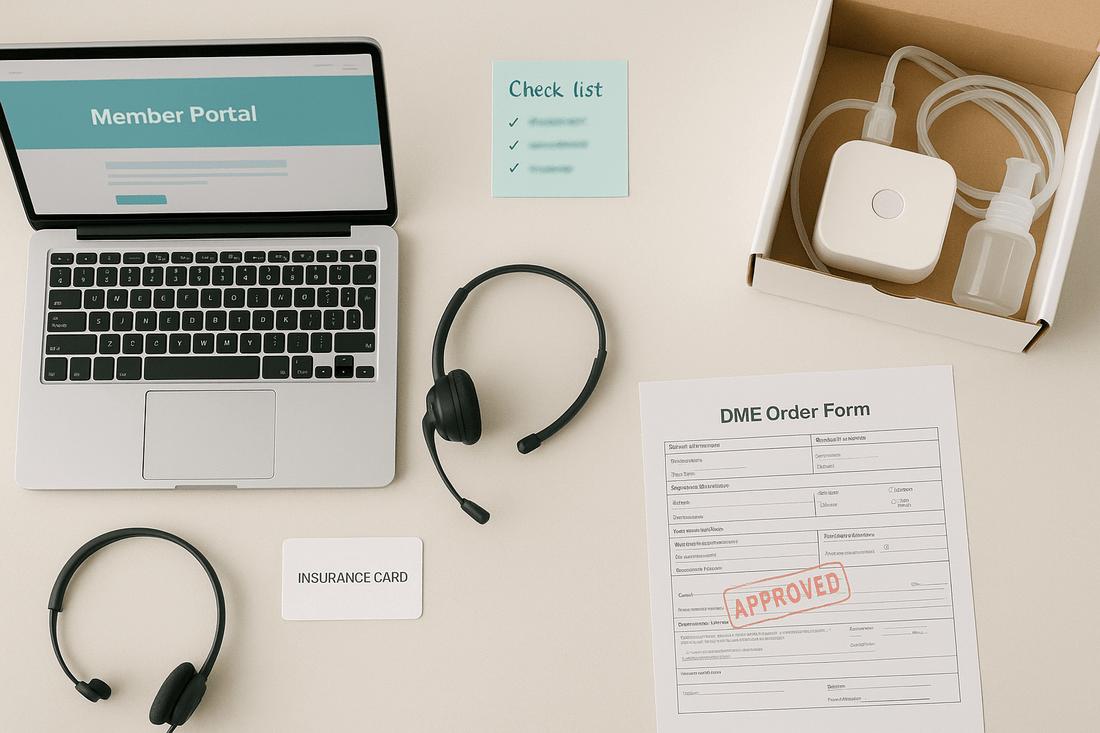
Ordering step-by-step (in-network DME)

- Verify benefits: Call the number on your Aetna card or check your member portal to confirm eligibility, allowed pump types, and any Rx/prior-auth rules.
- Choose an in-network DME supplier: Use Aetna’s provider directory or member portal. In-network ensures correct billing and minimizes denials.
- Select your pump: Pick from the supplier’s Aetna-eligible list. If you want a premium upgrade, ask for the out-of-pocket difference upfront.
- Submit documents: Share your member info, due/birth date, and—if needed—your prescription. The DME confirms coverage with Aetna.
- Shipping & tracking: Once approved, your pump ships directly to you. Save the packing slip and order confirmation.
- After delivery: Check the EOB (Explanation of Benefits). If you see unexpected charges, contact the DME and Aetna right away to correct coding or network issues.
Timing, replacement intervals & upgrades
Many plans allow ordering during pregnancy or after delivery; some restrict replacement of an electric pump to once every set interval (e.g., 12 months) or once per pregnancy. Supply kits may be covered once per pregnancy or at specific intervals. If a wearable or premium model is your preference, ask for an upgrade quote—Aetna pays the allowed amount; you pay the difference to the DME.
Hospital-grade rental (when it’s covered)
Hospital-grade rentals are typically reserved for medical necessity—for example, when a newborn remains hospitalized/NICU or when specific clinical criteria are met (low milk transfer, certain maternal/infant conditions). Your clinician and the DME coordinate documentation. Approvals are usually time-limited and may require renewals at set intervals.
Costs, common denials & how to avoid them
- Out-of-network DME: Using a non-contracted supplier can trigger denials or higher coinsurance—stick to in-network unless pre-approved.
- Missing Rx (when required): If your plan requires a prescription and it’s not on file, claims may deny. Ask your provider to e-fax it to the DME.
- Duplicate within interval: If you received an electric pump within the plan’s replacement window, a new one may not be covered—consider supplies only or pay upgrade cost.
- Upgrade misunderstandings: Clarify the allowed amount vs. cash price and your exact out-of-pocket before checkout.
- Appeals: If denied, review your EOB, request the claim notes, and file an appeal with supporting documents (Rx, NICU notes, clinician letter). Keep names, dates, and reference numbers.
Lactation support & work accommodations
Many Aetna plans include counseling with in-network providers (e.g., IBCLCs). For returning to work, federal rules generally require reasonable break time and a private space (not a bathroom) for pumping. Ask your HR team about a lactation room and cold storage access; bring a small cooler with ice packs for transport.
Comfort between sessions
Soreness from early pumping is common and often improves with correct flange size, gentle levels, and short warm compresses. Between sessions, some parents like reusable silver nursing cups for surface tenderness—always remove before nursing or pumping. Refresh valves/diaphragms regularly to maintain suction and efficiency.
FAQ
Do I need to wait until delivery to order?
Not always. Many plans allow ordering during pregnancy; confirm your timing window and any Rx requirements with Aetna and your DME.
Are wearable pumps covered?
Coverage varies. Standard electric/manual pumps are typically covered in full; many plans allow paid upgrades to premium wearables through in-network DMEs.
Will Aetna cover a second pump for work?
Usually not within the replacement interval. Some plans cover supplies or a manual pump; check your SBC for exact limits.
Can I rent a hospital-grade pump if my baby is in the NICU?
Often yes, for the duration of hospitalization or while medical necessity persists—coordinate documentation with your clinician and the DME.
What if I’m on a self-funded employer plan?
Benefits may differ from standard Aetna policies. Always verify directly with Aetna Member Services and your HR benefits team.


